Professor Juliana Chan: The Impact of CGM on Emotions and Behavior | 2025 DDMC
On June 7, 2025, the 2nd Digital Diabetes Management Conference was held in Chengdu, Sichuan. Against the backdrop of globally suboptimal glycemic control, Professor Juliana Chan from the Department of Medicine and Therapeutics at The Chinese University of Hong Kong delivered a presentation titled “The Impact of CGM on Emotions and Behavior.” This article summarizes the key insights from her presentation for reference.
Multifactorial Influences on Diabetes Management
1. Physiological and Behavioral Factors
Glycemic fluctuations in people with diabetes are influenced by multiple factors, including insulin secretion, blood glucose levels, medication, diet, physical activity, major life events, weight changes, stress, and sleep.
The ADA guidelines emphasize 24-hour behavioral management, which includes maintaining good sleep quality and regular sleep patterns, avoiding prolonged sedentary behavior, achieving sufficient daily step counts, and engaging in muscle-strengthening activities. Notably, insufficient sleep can significantly increase glycemic variability.
2. Psychological and Emotional Factors
Depression and Anxiety:
Studies in China have shown that the prevalence of depression among people with diabetes ranges from approximately 14% to 40%, and is associated with factors such as age, BMI, insulin use, and disease duration. Korean studies have confirmed that CGM combined with psychological interventions can help improve patients’ emotional well-being and metabolic indicators (e.g., lipid profiles, insulin resistance).
3. Discrepancy Between Subjective Perception and Objective Data
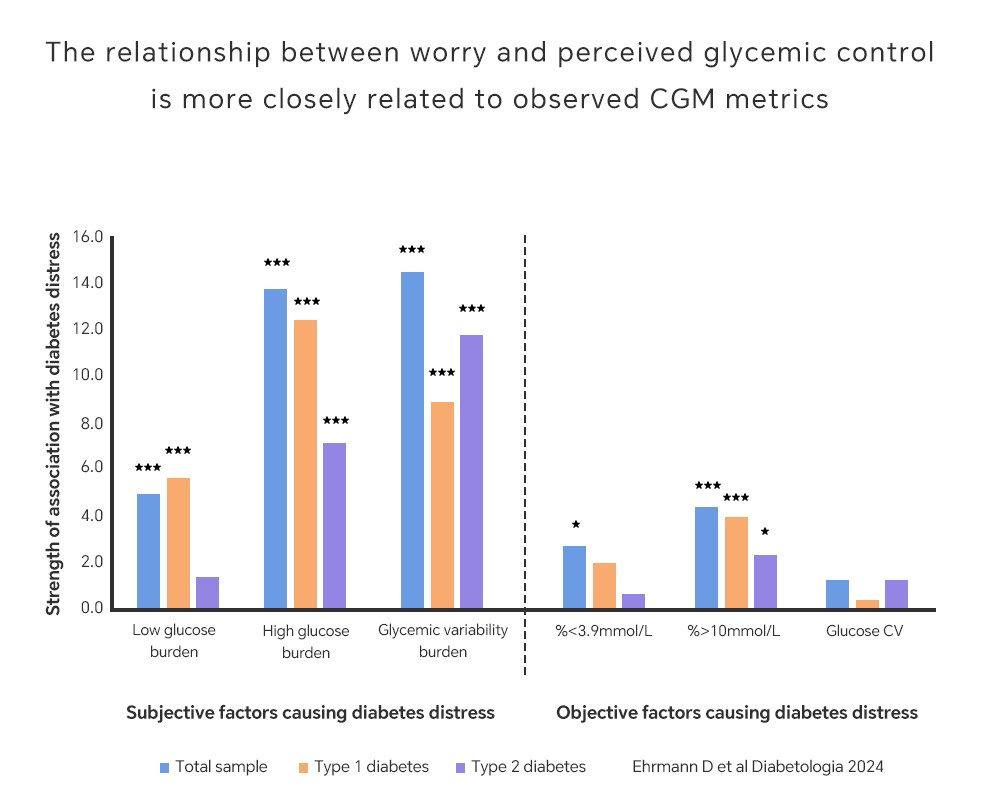
In a study involving 379 people with diabetes (50% with type 1 diabetes), researchers collected patients’ real-time subjective feelings via an app while continuously monitoring their glucose levels with CGM over 17 days. Results showed that patients’ subjective perception of glucose control played a more critical role in diabetes-related psychological distress than the objective data itself. Although CGM-derived data had a weak direct correlation with psychological distress, it was associated with better mental health overall. This finding underscores the importance of addressing patients’ subjective experiences in clinical management.
Role of CGM in Diabetes Management
1. Enhancing Awareness and Facilitating Behavioral Interventions
CGM provides real-time glucose data that helps patients directly understand the relationship between glucose fluctuations and daily habits (e.g., physical activity, sleep), thereby raising health awareness. For example, Korean studies have shown that CGM interventions can boost patients’ self-efficacy and reduce stress and depressive symptoms.
Digital interventions (such as CGM combined with apps) can improve health literacy and glycemic control, with notable benefits in hypoglycemia warning and prevention.
2. Personalized Management and Precision Medicine
CGM data supports stratified diabetes management. For example, patients can be categorized by sleep quality (sufficient / insufficient / severely insufficient), physical activity patterns, and hypoglycemia risk to develop targeted intervention plans.
Long-term follow-up shows that glycemic stability (e.g., Coefficient of Variation, CV) is an independent predictor of diabetes complications and mortality. CGM can help optimize the management of glucose variability.
Bidirectional Relationship Between Emotions and Glycemia
1. Impact of Emotions on Blood Glucose
Emotions such as depression and anxiety indirectly affect glycemic control by influencing diet, physical activity, and medication adherence, and are linked to increased risk of hypoglycemia (e.g., depressed patients are more prone to asymptomatic hypoglycemia).
Stress and insufficient sleep can directly worsen glycemic instability through physiological mechanisms such as dysregulated hormone secretion.
2. Impact of Glycemic Variability on Emotions
The unpleasant experience of hypoglycemia (e.g., anxiety, fear) may lead patients to deliberately maintain higher glucose levels, creating a psychological burden. Frequent glucose fluctuations increase diabetes distress and reduce quality of life.

By providing real-time dynamic monitoring, CGM not only offers a scientific basis for glycemic management but also lays the groundwork for personalized and precise psychological interventions. It helps identify and address patients’ psychological burdens and behavioral patterns, promoting a more holistic, patient-centered approach to diabetes management.
